…That is the Kawaquestion!
If you’ve been following Freya’s Story through my blog or on Facebook (www.facebook.com.freyasstory), then you’ll know that one of the hurdles I have been trying to get over since her diagnosis and treatment for Kawasaki Disease is the question of when to immunise. When is the important question here – it is not a question of ‘if’ for me. Freya is my 3rd child; I had the older two vaccinated in line with the standard UK immunisation schedules without hesitation. They both had the (then controversial) MMR vaccination that was vilified for years, for those claims to be later contradicted by the very doctor who made them. I am not an antivaxer (yes, that is a word that is banded around various mum networks). I can’t say I’m a provaxer either to be fair; in all things medical I am a conformist. I trust the NHS and the doctors to have made the right decisions. Well I used to anyway.
Now before I go on to share all the information I have in relation to this subject, there are a couple of things you should know. First of all, the information I have received is contradictory to say the least. I’ve even had different information from the same doctor, just on a different day. And therein lies one of the biggest issues, and the key reason why we should be campaigning for standard protocols for treatment and care of Kawasaki patients. But that’s a whole other blog. Secondly, I take no responsibility for the decisions you may make in relation to this issue. I am not a medical professional; I am just a mum that wants to do the right thing for her child. I could not protect my baby from Kawasaki Disease; I have to be able to protect her from the other nasties, if I can. I will share the information I have and where I’ve found it. You also need to understand that Freya’s case is an individual one. We certainly haven’t found a doctor in the UK who has received a patient as young as Freya where Kawasaki’s is concerned. Generally children are older (commonly between 6 months and 5 years) and have therefore already begun their immunisation journey. Infants diagnosed with this disease have often already had at least the first tranche of jabs (leading some to believe the vaccine to have been the trigger that KD needed to start it’s evil – a theory that I don’t discount, in fact I find it a very interesting theory with some validity and would not be surprised if it is confirmed as one of the triggers in the not too distant future). Indeed, some of the vaccines state an increased risk of Kawasaki Disease in the patient information – information we often don’t read before we give consent for the needle to go in. Again, I do not want to be a scaremonger, and it is absolutely not my intention to send cats amongst pigeons. I’ve already said I am a provaxer. I am pro-choice in all things – but I believe in those choices being informed if you are someone like me who needs to know it all (and often thinks she does, lol!).
Freya was 7 weeks old when she became sick. She was hospitalised on the very first day that she showed a single symptom (fever) and spent a number of days on a paediatric HDU, several weeks in a Children’s Hospital, and a week on a Cardiac HDU. We hadn’t yet seen a health visitor, and the appointment for her first set of immunisations (8 weeks) has just come through. I guess due to her condition, and later the treatment she received, it wasn’t possible to start the process of vaccinating with Freya whilst she was in the hospital. She was 7 weeks old when she went in, and 13 weeks when she came out, so she was already behind schedule. She received a blood transfusion, intravenous immunoglobulin (a blood product) and intravenous and oral steroids. All of these have an impact on the immune system, rendering vaccination difficult for a certain period of time. And I can’t be more specific than that, because that is one of the biggest areas of contradiction I have come across when researching this subject, and the reason why now, at nearly 10 months old, Freya has not had a single vaccination.
Some might wonder why that is an issue. Plenty of parents (those antivaxers) make the decision not to immunise their children against some or even all of the diseases that the immunisation schedules seek to protect them from. There are children who are unable to receive the immunisations because of poor, weakened or non-existent immunity. We vaccinate the many to protect the few; herd immunity. I could trust that everyone else has been protected, so Freya will be ok among the herd. But, what if… And then there is chicken pox – we don’t routinely vaccinate for that here in the UK (they do in the States). If you Google “chicken pox and aspirin” you will find one big reason why aspirin and kids don’t mix; Reye’s Syndrome, a rare but potentially fatal illness linked to the fever associated with Chicken Pox and Influenza in children taking aspirin. Ok, so the link has been found where high doses of aspirin are taken, and not yet with the low anti-platelet doses that a KD kid is prescribed, but nonetheless it’s a nasty illness and one I don’t want to take any chances with. Freya has been through enough.
So what happens if you have a child who has not been immunised, and you are concerned about them coming into contact with what others would consider pretty innocuous illnesses? Let me tell you what happens with us. Freya has not been to a baby group; not baby massage, or baby music, or baby yoga. Hell, she hasn’t even been to a playgroup, and when my older two get invited to a kids party, Freya stays at home. Don’t get me wrong; we have not become social recluses. Instead I apply my common sense to the activities we will undertake. I know there might be someone in the coffee shop who has the flu. Why is that kid in the shopping centre not at school? Could they have chicken pox? I can’t hide us away from the whole world, but I can reduce the risk of her coming into contact with these nasty germs and bugs. I call it damage limitation. She has one or two little friends that she sees from time to time, but only when they are well. And don’t forget she has an older brother and sister who are exposed to all manner of things at school every day – we don’t make them wear a mask! It is a source of sadness for me though. Freya is such a happy, sociable child, and I worry about the effect this lack of exposure to her peers might have on her development. I want her to laugh and play with other children, to learn how to share, to grow bonds and discover new things. Instead there is a lot of singing and dancing going on in this house, which isn’t a bad thing (unless you’ve heard my singing!!). And with a bit of luck we can catch up with those immunisations soon and provide what we believe to be a little protective bubble around our child before it is too late for her to start over. The knock-on effect of KD will be huge – when I return to work, she will have to go to some form of childcare. She will be over a year old, and will never have been with anyone else other than her close family. That’s going to be a tough one for both of us to handle…
Let me go back to the beginning of Freya’s immunisation journey. While we were in the hospital with Freya we were advised that she shouldn’t have the immunisations, first because of her condition, and secondly because of the medication. A lady used to pop her head in our cubicle door every other day with an immunisation leaflet and I repeated often that we had been advised Freya would have to be left to catch up. I was promised an individualised immunisation schedule to leave the hospital with; it never materialised. I made a number of calls to the hospital to enquire about when I could start the process, and to the Health Visiting team to ask them to stop the weekly postal reminders telling me what I already knew; Freya had not received her first immunisations. Eventually I got the call from the hospital that advised I could give her any killed (inactive) vaccinations immediately (she was discharged one month after treatment for KD), but that I should wait 3 months post steroid treatment for any live ones.
I did a bit of research, because I was convinced there should also be a timescale for receiving vaccinations after a blood transfusion. All avenues confirmed that vaccinations should not be given until 6 months after a transfusion. Not to mention the varying timescales quoted for giving vaccinations after IVIG! But all my hospital ever referred to was the steroid treatment, I guess because that is an immuno-suppressant. But what of the other things? Had they forgotten what she had been given? I felt uneasy with the advice, so I sat on it for a while.
At a follow-up appointment with Rheumatology, I asked about whether Freya should be vaccinated against Chicken Pox (Varicella). The doctor said that in the UK we only vaccinate children who are at high risk of contracting the disease. I said that whilst Freya wasn’t at higher risk of contracting chicken pox, the potential consequences of her contracting the disease whilst taking aspirin could be catastrophic. He agreed to take the issue away, and on the 19th August 2015 I received a letter confirming that they believed it was “reasonable for Freya to receive vaccination against Chicken Pox, both in relation to the issue regarding ongoing treatment with aspirin and the small degree of risk of developing [RS] and also the small risks that Freya may require treatment with immunosuppression therapy in the future…”. Freya had been weaned off steroid therapy a lot more quickly than originally planned when the gastrointestinal bleeding started. From memory, it was the 8th July 2015 when she took her last oral prednisolone; that meant she could have the live vaccines, including CP, anytime after the 8th October 2015; “…it is important that Freya does not receive this until at least 3 months following…the last day Freya received the steroid treatment…”. I still felt uneasy, and decided to wait until our next follow-up appointment to discuss. It was at that appointment that I shared all the research that I had done, and got a referral to Immunology. I had to wait until yesterday for that appointment.
I wonder if now might be a good time to share what I have learned, from the internet (reliable sources, like the NHS and the American Heart Association) and from medical professionals from London to California…
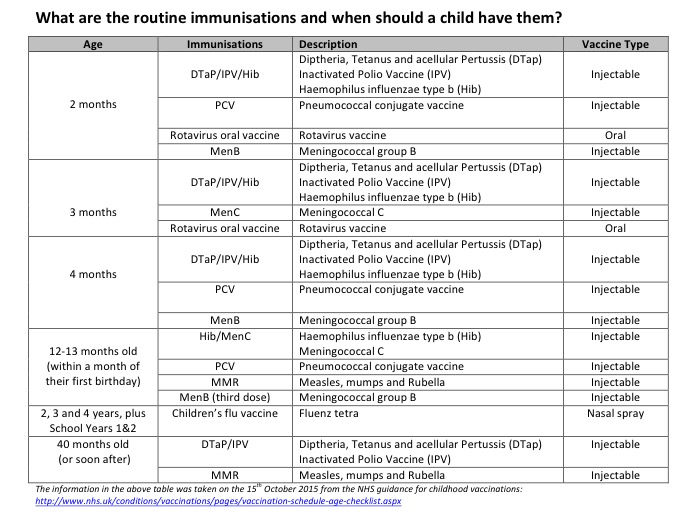
From the list above, all vaccines are inactive with the exception of the following live vaccines – Rotavirus, MMR, Children’s Flu vaccine (note that for the children’s flu vaccine, the nasal spray is live, however there is an injectable inactive flu virus available).
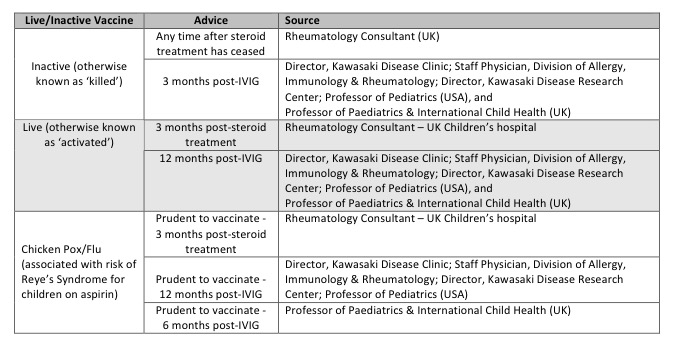
These are just a few examples of the responses I received from medical professionals, and I can say that my internet research has thrown up much the same; anything from 3 months to 12 months. Helpful, right! My gut feeling was telling me I should err on the side of caution, and follow the advice of the US doctor who is considered the leading Kawasaki Specialist in the World – she calls herself a ‘Kawasakiologist’ and I believe she deserves the title. Our GP agreed that Freya qualified for the injectable (inactive) flu vaccine. My decision was made. Well, kind of. I had decided I wanted to get Freya caught up on the inactive vaccines immediately, then discuss the issue of the live ones with our Immunologist. Chances were, by the time we got any decisions we would be nearing that 12 month mark anyway, so it was a win-win. But our ever cautious GP decided that if we were speaking to an Immunologist anyway, there was no harm in waiting for that meeting before we started the immunisation process, and he felt happier to wait for clear direction from her. So, again we would have to wait.
So yesterday we had that appointment with the Immunologist. I was all geared up to go in and cover all my questions, but unfortunately an hour’s wait with a baby that has decided that a high pitched squeal is the best means of communication made the whole process a little trickier than I had anticipated! The doctor was the Infectious Diseases Consultant who treated Freya when she arrived at the Children’s Hospital on day 8 of her illness. That was nice, as I had the opportunity to thank her for her compassion, support and tireless determination to get to the root of Freya’s condition (especially as I was quite a difficult ‘customer’ who asked lots and lots of questions, and even accused them of breaking Freya’s heart at one point!) She seemed genuinely pleased to see Freya looking so well. She received the news that we had seen some improvement in her coronaries since the acute stage of the illness with a broad smile, and she was happy that Freya has not had anything more than one little cough and cold since her hospitalisation. I expected her to call me a muppet for being a cautious and over-protective mother, but instead she said she felt I was doing the right things, which was reassuring.
I came away from the appointment with a solution, individualised for Freya. I still don’t have a definitive answer about the timescales related to immunising after IVIG. But then why would I? The fact that I can quote at least 5 different timescales from medical papers and journals across the world tells me a lot of them are guessing. I’ve read that medics aren’t completely sure why IVIG even works in the case of KD – they are still trying to understand what causes the illness in the first place, so I guess it would be near impossible to understand why the treatment works. It just does (in most cases). The Immunologist told me that they deal with children who have compromised immunity as a result of a bone marrow transplant, for example. Those children are given immunisations in line with the hospital guidelines and they do not wait 12 months. That said, she agreed that they had learned more than they previously knew about KD from Freya. Presenting at just 7 weeks old, and having had no previous immunisations, she is a bit of an unusual case. So they have agreed to follow a similar process to that of a bone marrow transplant patient.
What are they going to do?
They have taken blood samples from Freya in order to test her body’s immunity status. They will be testing Freya’s immunoglobulin levels, and lymphocytes (T-cells). Depending on those results (and I am sorry, I didn’t ask what result they would be expecting or what a low or high result might indicate, or whether there was a chance they might just be reading ‘borrowed’ antibodies as a result of the circulating IVIG – I will ask that when we discuss results), they will start the routine inactive vaccines and the injectible (inactive) flu vaccine. After a period of time following those (I think she said 6 weeks), Freya’s immunoglobulins will be tested again to check her immune response to those vaccines. Assuming they get the right result (whatever that might be), they will then progress to live vaccines, including chicken pox. If we get moving quickly, Freya may even make it in time to have the MMR vaccination at precisely the right time. I have some decisions to make about Rotavirus (which I believe is time-specific so she may already be considered too late) and Meningitis B, as both have stated increased risks of contracting Kawasaki Disease in the patient information. I know it is incredibly rare for KD to reoccur, but show me one parent of a kid with a rare condition who finds that word reassuring.
Yes, I am still confused as to what the right answer is about timescales for vaccinations post treatment Kawasaki Disease. But, I think I have a great solution for me, for Freya. Rather than guess based on the varied guidelines out there, we are going to take a look at Freya as an individual. Actually take a look inside and see what is going on, and make the decisions based on what she tells us. The Immunologist has always said that Freya showed them the path to a diagnosis, and that they learned so much from her. Seems she is going to teach them something new. And as much as I probably do their heads in with my questions and powerpoint presentations, I do know that they respect me for it and that they are luckily not too arrogant as to discount this mum’s research and opinions. She actually said it was helpful and told Freya that she is as well as she is because of her “amazing mum”. I don’t know about that, but in a sea of negativity and low moments, I’ll take that right now.
Whatever I learn from this experience, I will share. Every Kawasaki case is different, no matter how similar some of the stories might seem. No wonder it is a tricky one to spot, diagnose, treat and understand. I hope in my lifetime they find the cause so I can finally understand why this happened to us, to my little Peanut.
Our Rheumatologist said that the subject of immunisations in these cases is “contentious” and currently being debated. Another said that “guidance is not clear as there are no trials/studies to guide us for this exact situation…” and “…is a balance involving unknowns…” He gave his opinion and advice, stating that “…there are other equally ‘correct’ versions too!” No shit!
I’ll leave you with a few of the comments that I received from KD specialists here and in the US, which might help to dispel a few myths relating to IVIG and immunity.
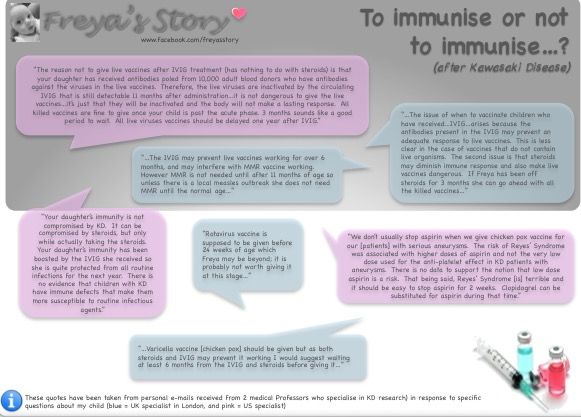
And in case you can’t read that, I have pasted below:
“The reason not to give live vaccines after IVIG treatment (has nothing to do with steroids) is that your daughter has received antibodies poled from 10,000 adult blood donors who have antibodies against the viruses in the live vaccines. Therefore, the live viruses are inactivated by the circulating IVIG that is still detectable 11 months after administration…it is not dangerous to give the live vaccines…it’s just that they will be inactivated and the body will not make a lasting response. All killed vaccines are fine to give once your child is past the acute phase. 3 months sounds like a good period to wait. All live viruses vaccines should be delayed one year after IVIG.”
“We don’t usually stop aspirin when we give chicken pox vaccine for our [patients] with serious aneurysms. The risk of Reyes’ Syndrome was associated with higher doses of aspirin and not the very low dose used for the anti-platelet effect in KD patients with aneurysms. There is no data to support the notion that low dose aspirin is a risk. That being said, Reyes’ Syndrome [is] terrible and it should be easy to stop aspirin for 2 weeks. Clopidogrel can be substituted for aspirin during that time.”
“Your daughter’s immunity is not compromised by KD. It can be compromised by steroids, but only while actually taking the steroids. Your daughter’s immunity has been boosted by the IVIG she received so she is quite protected from all routine infections for the next year. There is no evidence that children with KD have immune defects that make them more susceptible to routine infectious agents.”
“…The issue of when to vaccinate children who have received…IVIG…arises because the antibodies present in the IVIG may prevent an adequate response to live vaccines. This is less clear in the case of vaccines that do not contain live organisms. The second issue is that steroids may diminish immune response and also make live vaccines dangerous. If Freya has been off steroids for 3 months she can go ahead with all the killed vaccines…”
“…The IVIG may prevent live vaccines working for over 6 months, and may interfere with MMR vaccine working. However MMR is not needed until after 11 months of age so unless there is a local measles outbreak she does not need MMR until the normal age…”
“Rotavirus vaccine is supposed to be given before 24 weeks of age which Freya may be beyond; it is probably not worth giving it at this stage…”
“…Varicella vaccine [chicken pox] should be given but as both steroids and IVIG may prevent it working I would suggest waiting at least 6 months from the IVIG and steroids before giving it…”








